The True Cost of a Diagnosis: What Nobody Tells You About Paying for Autism Support
We thought the appointment was the finish line. It was just the starting gun.
When your child is diagnosed as autistic, you don’t just walk out with answers. You walk out with a multi-thousand-dollar to-do list, a flood of paperwork, a part-time job in navigating systems, and a gnawing fear about what happens if you can’t afford what they say your kid needs.
Take Emily and James. Their son was diagnosed at 3. They had decent insurance, a modest emergency fund, and flexible jobs. They thought they were ready. Six months later, they’d drained their savings, maxed a credit card, and were taking alternating days off work to cover therapy appointments. A year in, they sold their second car to keep paying for support. The diagnosis cost represented just 4% of what they’d spend in the first year alone.
"We could handle the diagnosis. We couldn’t handle the paperwork, the denials, the hours on hold with insurance companies who seemed determined to wear us down."
The Visible Costs: What You Expect to Pay
Most caregivers brace themselves for the upfront expenses:
- Developmental pediatrician or pediatric neurologist: $600–$1,200 per visit
- ADOS or cognitive assessments: $1,000–$3,000 depending on location
- Speech/language evaluations and psychological testing: $300–$1,000
For context, these initial diagnostic costs typically represent 3–8% of the median U.S. household income of $70,000. Even with insurance, many specialists are out-of-network or involve long delays. Waitlists become their own kind of cost—delaying therapy often means paying significantly more later as children age out of early intervention programs.
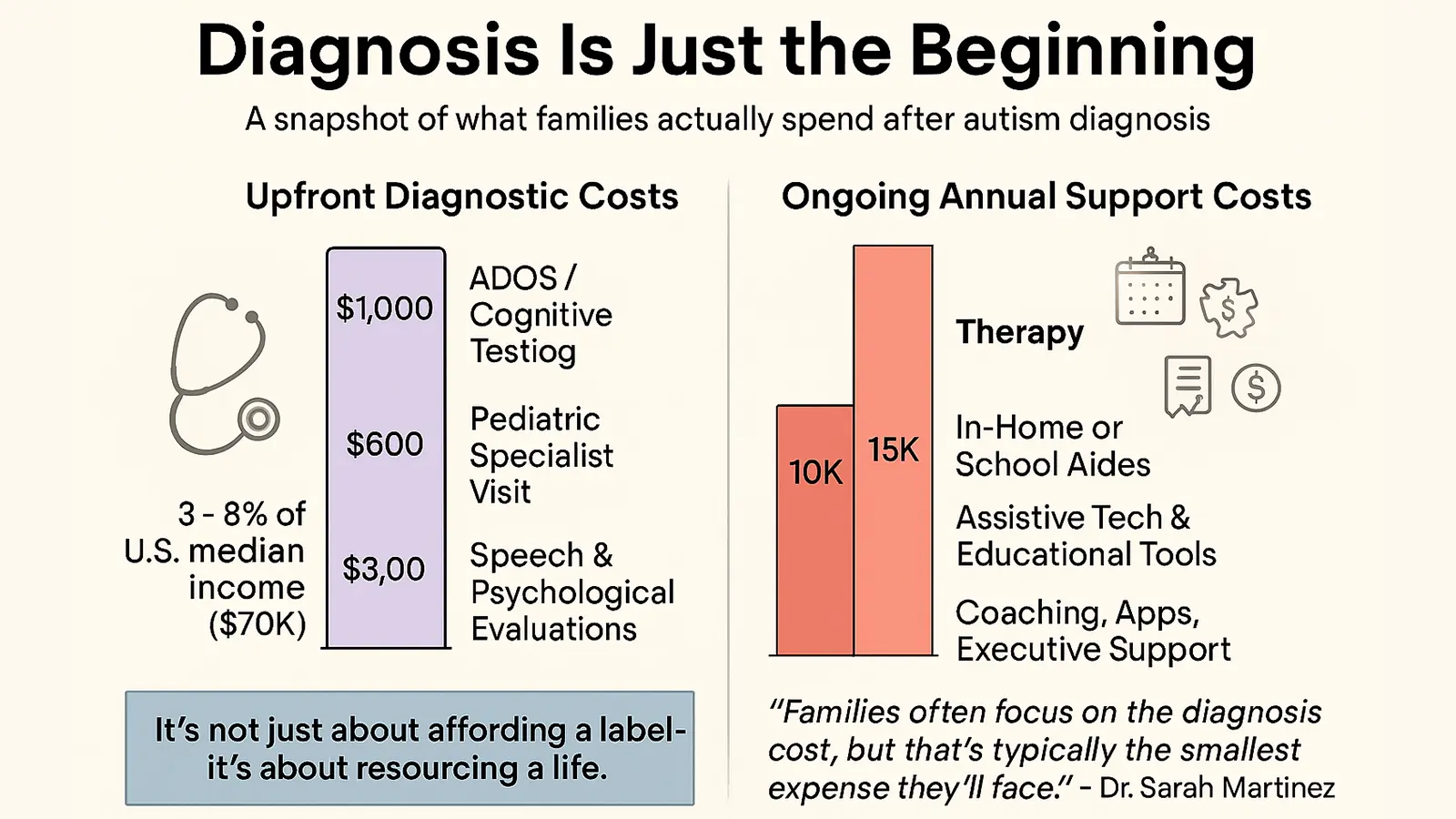
Dr. Sarah Martinez, a developmental pediatrician in Austin, explains: "Families often focus on the diagnosis cost, but that's typically the smallest expense they'll face. The ongoing support costs can easily reach $50,000–$100,000 annually for comprehensive services."
The Invisible Costs: The Avalanche Afterward
Here’s what no one tells you: the expenses keep stacking after the diagnosis.
Direct Therapy Costs:
- Speech therapy: $75–$150/session (1–3x weekly = $300–1,800/month)
- Occupational therapy: $100–$200/session (1–2x weekly = $400–1,600/month)
- ABA or other behavioral supports: $1,200–$2,500/month for 10–20 hours weekly
- Specialized evaluations and reassessments: $500–$2,000 annually
Hidden Ongoing Expenses:
- AAC devices ($3,000–$8,000), weighted blankets, noise-cancelling headphones
- Private tutoring, educational advocates, special school placements
- Medications, emergency visits, co-pays, and labs
Opportunity Costs:
- Lost work hours, reduced career advancement
- Childcare for siblings during therapy
- Burnout-related medical and mental health care
- Transportation, gas, and time off for multiple weekly appointments
“We started rationing therapy—one week on, one week off—because we couldn’t keep up with the $800/week cost.”
Combined, these costs can easily reach 25–40% of a household’s annual income.
“I Wasn’t Ready For…” – Real Parent Voices
"I wasn't ready for the guilt of not being able to afford 20 hours of ABA a week that the team said my daughter 'needed.'"
"I thought diagnosis meant we'd finally get help. Instead, I had to become an expert in five systems overnight while working full-time."
"The emotional cost of fighting insurance denials while watching your child struggle is something no one prepares you for."
ND Parents Raising ND Kids: The Double Tax
If you're neurodivergent yourself? Everything hits harder.
Executive dysfunction, sensory fatigue, and shame spirals don’t mix well with appeals paperwork, early-morning appointments, and confrontation-heavy advocacy. The cost isn’t just financial—it’s cognitive and emotional.
"I couldn’t figure out how to apply for the help they told me existed. I’d freeze every time I opened the application. My executive function was already maxed out."
You're managing your child’s needs—and your own burnout—inside systems designed for neurotypical minds.
Divergent Money Types—What You Might Experience:
- Overstimulated Avoiders: Sensory overload from clinics, forms, and phone calls
- Systems Hackers: Excellent at research, struggle with consistency
- Money Ghosts: Financial trauma resurfaces when costs spiral
- Turtles: Avoid finances entirely as a shutdown response
What Helps (Even a Little)
This system is broken—but there are cracks where sunlight gets through.
Low-Effort, Quick Impact:
- Ask every provider about sliding scale or scholarships
- Use university training clinics or nonprofits for discounted therapy
- Maximize HSA/FSA use; many expenses qualify
Moderate Effort, Medium Payoff:
- Apply for grants: UnitedHealthcare Children’s Foundation, Autism Care Today
- Request a case manager from your insurance company
- Document every interaction and denial
High-Effort, High Impact:
- Learn how to file formal appeals (40% win on first appeal)
- Explore Medicaid waivers, SSI, and early intervention mandates
- Open an ABLE account or begin a Special Needs Trust
Can't Afford Any of This? Start Here.
- Free school district evaluations
- Early intervention services (0–3), regardless of income
- University therapy training programs
- Local churches and United Way 211 financial assistance
How Geography and Demographics Impact Care
| Factor | High-Income Urban | Low-Income Rural |
|---|---|---|
| Diagnosis Cost | $2,500–$5,000 | $1,000–$2,000 |
| Provider Access | High | Low, long travel times |
| Waitlists | Shorter | Often 12–24 months |
White children are diagnosed 1.6x more often than Black children.
Higher-income families access services 2–3 years earlier, on average.
How the U.S. Compares
| Country | Average Diagnosis Cost | Therapy Coverage | Waitlist Time |
|---|---|---|---|
| U.S. | $1,500–$4,000 | Patchwork | 6–18 months |
| Canada | $0–$1,000 | Provincial | 12–24 months |
| UK | Usually free (NHS) | Limited | 18–36 months |
| Australia | $500–$1,500 | Medicare Partial | 6–12 months |
| Germany | €0–€500 | Full | 3–6 months |
Managing the Emotional Cost of Financial Stress
- Guilt about “not doing enough” is common—despite doing everything you can
- Marriage strain: Over 70% of parents say financial stress impacts their relationship
- Burnout from system navigation is real—consider therapy, support groups, or time-blocked paperwork hours
FAQs About Paying for an Autism Diagnosis
Q: Is autism testing covered by insurance?
A: It varies. Pre-authorization is often required. Testing may only be partially reimbursed.
Q: How much does an autism evaluation cost out of pocket?
A: Between $1,000 and $4,000, depending on location and scope.
Q: Are there grants to help pay for therapy?
A: Yes—many national and local programs offer $500–$5,000.
Q: Can I deduct autism-related expenses on taxes?
A: Yes, if they exceed 7.5% of AGI. IRS Form 502 applies.
Q: What if I can’t afford what my child “needs”?
A: Prioritize the most effective services first. Use public school, free early intervention, and community-based help.
You’re Not Failing. You’re Carrying Too Much Alone.
You didn’t just get a diagnosis. You got a job—unpaid, overwhelming, and invisible. You're now the care coordinator, the financial strategist, the legal advocate, the meltdown whisperer. That’s not a personal failing. That’s a broken contract.
Because the truth is: autism isn’t the cost. The infrastructure around it is.
Families don’t fail. They burn out under the weight of delays, denials, and systems that assume unlimited time, money, and self-sacrifice.
Here’s what that cost actually looks like:
- When insurance delays services by months—that’s a cost.
- When schools fight against supports—that’s a cost.
- When therapy coverage runs out mid-year—that’s a cost.
- When your income drops because you can’t be in two places at once—that’s a cost.
And they’re all invisible on a diagnosis form.
So What Now?
You deserve more than awareness. You deserve structure, support, and breathing room.
Here’s what we advocate for:
- Universal early intervention through age 8
- Mandatory therapy coverage parity, with no loopholes
- Schools trained to work with neurodivergent families—not against them
- Financial aid for caregiver support and long-term planning
And Here’s What You Can Do Right Now:
🫱 Share this article with someone who needs to understand the real cost.
Not just the diagnosis—but the daily, compounding cost of being unsupported.
📣 Talk about this. Loudly. Kindly. Repeatedly.
Policy doesn’t change until enough people say, “This isn’t working.”
One Last Thing:
You didn’t fall behind.
You’ve been carrying the weight of two people in a system built for one.
And you’re still here.
That’s not failure. That’s strength under pressure.
Let’s start stacking wins, together.
Want financial strategies that match your neurodivergent brain?
Take our Divergent Money Matrix Quiz.
Disclaimer: As ALWAYS, this article is for educational and motivational purposes and is not financial advice. Always consider consulting with a financial professional for guidance tailored to your unique situation.